The clinical consequences of trisomy 8 (+8) are reflected by its categorization as an intermediate risk cytogenetic abnormality in AML while in MDS it has a more favorable impact. Gain of chromosome (chr.) 8 is a frequent event in other hematologic disorders and its prognostic role seems to be dependent on disease context. Some molecular lesions ( RUNX1, ASXL1) are distinctive of +8 AML and important in delineating its clinical phenotype and prognosis. However, the intrinsic molecular drivers contributing to clonal pathogenesis of myeloid neoplasia (MN) as repercussion of gain of chr.8 remain unclear. We stipulated that the study of clinical, genomic, and transcriptomic features of +8 MN will provide important clues to the pathogenesis of +8 and help refine its clinical implications in a specific clinical context.
NGS and clinical data from a cohort of 3971 MDS and 3973 AML patients were reviewed, including normal karyotype MDS/AML (NK MDS or AML), isolated +8 (iso +8 MDS/AML), and non-isolated +8 (non-iso +8 MDS/AML). In addition, RNASeq data were available in a subcohort of patients (82: +8; 617 NK MDS). Expression of chr.8 genes was studied to unmask culprit genes in +8 MN.
Compared to NK-AML, iso +8 AML patients were older (76% aged >60 years, P= .0005) and had more dysplastic than hyperproliferative phenotype as they presented with lower WBC (median: 9.5 vs 15.2x10 9/L, P= .008) and platelet counts (median: 49 vs 64 x10 9/L, P= .0002). Iso +8 AML had higher percentages of secondary AML (sAML, 17 vs 11%, P= .001) arising from antecedent MDS (14 vs 9%, P= .002) vs NK AML. As expected, survival analysis showed iso +8-AML to have worse median overall survival (mOS) vs NK AML (20 vs 32 months, P= .0001). Yet, when sub-classifying AML based on disease ontogeny (primary vs secondary), a significant mOS difference was only seen in primary AML (21.5 vs 34.5 months, P= .0002; in sAML, 14.7 vs 24.3 months, P= .3).
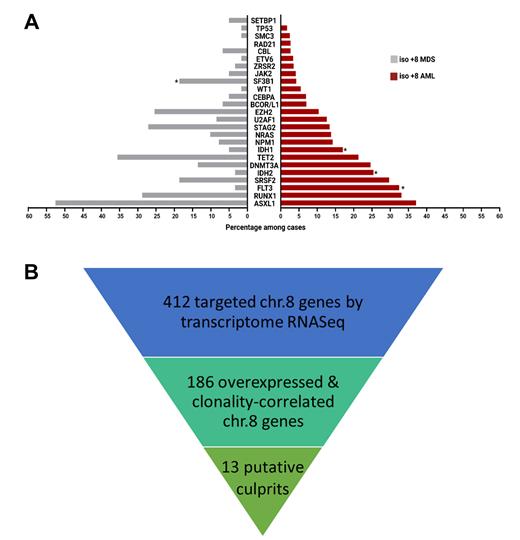
As for molecular associations, a variety of mutations were more frequent in iso +8 AML vs NK AML, including: lineage transcriptional factors ( RUNX1, 33 vs 17%, P< .0001), chromatin modifiers ( ASXL1 37 vs 13%, P< .0001; EZH2 10 vs 3.4%, P< .0001), splicing factors ( SRSF2 30 vs 13%, P< .0001; U2AF1, 12 vs 3%, P< .0001) and cohesin genes ( STAG2, 13 vs 7%, P= .02). In contrast, mutations in FLT3 (33 vs 42%, = .01), DNMT3A (24 vs 35%, P=.002), NPM1 (14 vs 44%, P<.0001) and CEBPA (7 vs 12%, P= .02) were more frequent in NK AML. We then focused on the iso +8 MDS vs NK MDS groups, and interestingly, found that ASXL1 (52 vs 19%, P< .0001), EZH2 (25 vs 4, P< .0001), RUNX1 (29 vs 12%, P= .0009), and STAG2 (27 vs 6%, P< .0001) were more frequently found in the +8 MDS compared to NK-MDS (similar patten to AML), whereas SRSF2 (19 vs 18%, P= .9) and U2AF1 (9 vs 6%, P=.7) were similar in both. The comparison of AML and MDS then showed that iso +8 AML was more commonly associated with mutations in FLT3 (33 vs 3%, P< .0001), IDH1 (17 vs 5%, P= .03), and IDH2 (25 vs 3%, P< .0001), while iso +8-MDS had higher odds of SF3B1 (19 vs 4%, P= .001) ( Fig1A).
We then investigated whether specific transcriptomic features may play a role in +8 MN pathogenesis by targeting the transcriptome of 412 chr.8 genes ( Fig1B). After adjusting for zygosity, we identified 186 genes correlating the change in expression levels with clonality. We further interrogated genes possibly eliciting oncogenic potential with log2 fold change (log2FC) ratio of at least 1.25 to reflect an extra chr.8 copy. We found higher mRNA expression levels of 13 putative culprit genes of known oncogenic potential in iso +8 MDS vs NK MDS including the anti-apoptotic protein BAG4 (LogFC 7.1 vs 5.4, P< .0001), possibly conferring growth advantage, toll-like receptor LY96 (LogFC 3.3 vs 2.0, P< .0001),the tyrosine protein kinase LYN (LogFC 8.4 vs 6.7, P< .0001), human oncogene WHSC1L1/NSD3 (LogFC 8.1 vs 6.5, P< .0001)and long non-coding RNA, PVT1 derived from an 8q24 intergenic region (LogFC 4.0 vs 2.2, P< .0001).
In summary, iso +8 MN represents a distinct entity defined by older age and dysplastic phenotype, likely due to genotypic enrichment in RUNX1 mutations, while inversely associated with proliferation genes ( e.g., FLT3 and NPM1 in NK). The key culprit oncogenes implicated in +8 MN may be located on the extra chr.8 itself. Indeed, we found transcriptomic changes pertinent to +8 MDS whose role in driving leukemogenesis and interaction with specific myeloid drivers needs to be confirmed by future experimentations on cellular and murine models.
Disclosures
Maciejewski:Regeneron: Consultancy, Honoraria; Alexion: Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria, Speakers Bureau; Omeros: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal